Labs enter the home stretch for implementing IQCP
By Steve Halasey
In August 2013, the Centers for Medicare and Medicaid Services (CMS) announced a new initiative for quality control (QC) in US clinical laboratories that would enable labs to implement an individualized quality control plan (IQCP). Based on the principles of risk management, the program provides labs with flexibility to customize their QC policies and procedures in accord with the test systems and unique characteristics of their facility.
CMS provided labs with a 2-year education and transition period, which will end when the IQCP program becomes fully effective on January 1, 2016. After that date, laboratories will no longer be able to use the equivalent quality control procedures previously permitted under the Clinical Laboratory Improvement Amendments of 1988 (CLIA).
By all accounts, the progress of US clinical laboratories toward implementation of individualized quality control planning has been slow and somewhat tentative. In this article, CLP looks at some of the issues that labs are considering, with an eye toward next January’s looming deadline.
PROGRESS REPORT
Although most labs seem not to have moved very far in the direction of implementing an IQCP, they haven’t been ignoring the opportunity. “The majority of laboratories are now aware of the approaching January 2016 deadline for implementing IQCP as an alternative QC option,” says James Liggins, president of COLA Resources Inc, Columbia, Md. “We are seeing an increase in labs reaching out for education and direction on implementing IQCP as the deadline approaches.”
Dixie Marshall, BS, MT(ASCP)SH, director of laboratory services at LifePoint Hospitals, Martinsville, Va, is among a small number of directors who have given their labs a head start. “I developed an IQCP plan and a template for our laboratory by November 2014,” she says. “The reason I did this early is that I wanted the Joint Commission surveyor to review the plan during our next survey. After I discovered that the surveyors did not do this, I invited the Joint Commission for a learning visit.”
More commonly, labs have made a beginning on the work needed to develop an IQCP plan for all of their tests, but they still have a lot more to do. “I have identified the test I need to have completed by January, set the priority list for the nonrequired tests for which I would like to have an IQCP plan, and started working on my first test,” says Christiane Nooney, MBA/MHA, MT(AMT), laboratory supervisor for the point-of-care testing program at Duke University Health System.
“I have drafted one IQCP, using a simple Excel spreadsheet format for documentation. I have not written any others since, however, awaiting the question of whether standardized IQCP template forms will be required by my accrediting organization,” says Valerie L. Ng, MD, PhD, chair of laboratory medicine and pathology at Alameda County Medical Center, Oakland, Calif.
“Standardized forms would serve two key purposes: an internal one to ensure the laboratory addresses all key issues in the entire test process; and an external one to ensure that laboratory inspectors will quickly recognize the IQCP and not waste time searching through a nonstandardized format.”
“I need to start completing my IQCPS beginning October 2015, as I think I’ll need 3 months to complete the entire process—draft IQCP for staff review, incorporation of staff-suggested comments and revisions, reality checking the revisions with testing personnel, then finalizing and implementing by January 1, 2016,” Ng adds.
But so far, few labs are so definite about the IQCP process or its timing. “Based upon what I am seeing out on survey, many labs are still confused and haven’t started working on IQCP,” says Elia Mears, MHA, MT(ASCP) SM, field representative for the laboratory accreditation program at the Joint Commission, Oakbrook Terrace, Ill. “Joint Commission laboratory accreditation program surveyors have received training about IQCP and they can direct organizations to resources and offer guidance, if needed.”
OBSTACLE COURSE
Despite the fact that labs are nearing the end of the 2-year transition period before final implementation of the IQCP rules, experts agree that progress has been slow. Individually and collectively, labs seem hesitant to begin the process without greater assurances about where it will lead them.
But it wouldn’t be fair to say that labs are entirely disengaged, either. “Our experience to date has shown that labs are seeking out the resources available to gain a better understanding of IQCP by attending workshops, contacting manufacturers, and looking to their accreditation or compliance organizations for information,” says Liggins.
To feel comfortable about moving forward with their IQCP planning, labs are seeking answers on a wide range of questions, says Liggins. Typical starting-point questions reflect the uncertainty that labs feel about the coming regime:
- Does my lab have to perform IQCP?
- What documentation will my inspector want to see in my files, and how should it be formatted?
- Should I perform IQCP on all testing (waived-, moderate-, and high-complexity)?
- How often should I perform an IQCP?
- What elements should an IQCP cover?
But even when companies have the right information at their fingertips, it may not be enough to break their logjam. “The biggest obstacle is that lab managers are being inundated with information and solutions from third parties, without clear, quantifiable, and logical direction from regulators,” says Zoe Brooks, principal of the laboratory quality consultancy Awesome Numbers, Toronto, ON, Canada.
The solution, says Brooks, is for labs to do the reading necessary to understand the new quality processes that the IQCP rules are meant to bring into play. “When labs understand the fundamental concepts and logic of risk management, most of its processes involve simple yes/no logic and black-and-white mathematics,” she says.
If labs had been able to execute such a simple solution before now, perhaps they would have already made greater progress on the path toward implementing IQCP. “It took me a lot of time to read and develop our IQCP,” says Marshall. “I think when new regulations are prepublished, CMS should send out examples of how to carry out the regulations.”
Moreover, with laboratory resources constrained and staff time at a premium, many lab directors are finding that performing an IQCP is just another permanent entry somewhere near the bottom of their “to do” pile. “Staffing shortages are certainly an obstacle,” says Mears. “It has been difficult for staff to get time away from the bench and daily tasks to learn about IQCP and work on their own plan.”
“Other issues with a higher priority are taking me away from the IQCP project,” agrees Nooney. “I’m doing what I can when I have a few free minutes. I have blocked out some time off later in the year—around October and November—to complete the process.”
“It’s always all about time and competing priorities,” agrees Ng. “I had planned on setting aside 2 hours weekly to focus on IQCP writing, expecting to complete an IQCP each week. But I’m finding that unplanned and of course urgent, time-sensitive projects have instead used this time such that I don’t have any ‘unused capacity’ to focus on IQCP writing.”
In common with many laboratory directors, Ng says that some of the most pressing and unexpected tasks requiring a significant amount of attention are external demands mandated by the Health Information Technology for Economic and Clinical Health (HITECH) Act and related information technology initiatives. In particular, satisfying requirements for electronic public health reporting, meaningful use of electronic health records, and the creation of a portal for distributing lab results to patients, are all time-consuming initiatives.
On top of such external demands, labs are not without their own time-consuming initiatives. Ng notes that her own time has also been drawn away by “huge internal projects related to moving into a new lab, coincident with implementing a robotic track system.
Put all these time-consuming demands together, and it’s no wonder that labs’ progress toward implementing IQCP has been slower than expected. But that’s not all.
“Because IQCP is based upon a lab’s individual risks, some people fear they might miss something in their risk assessment,” says Stacy Olea, MBA, MT(ASCP), FACHE, executive director of the laboratory accreditation program for the Joint Commission, Oakbrook Terrace, Ill. “They want to do it right the first time, so they’re spending time researching and looking for examples instead of getting started.”
But even a deliberate process populated with a lot of upfront fact-finding can have long-term benefits for labs. “Gathering information from the users and getting them involved is going to be a challenge, but worth it in the end,” says Karen Jenkins, MT(ASCP), POCC(AACC), point-of-care coordinator at Emory University Hospital, Midtown. “The relationships that are being cultivated during this period will prove to be very advantageous in the future.”
IMPROVING PATIENT CARE
IQCP represents a fundamentally different method of QC for clinical laboratories, imposing a risk assessment and mitigation approach on top of traditional QC testing procedures. The program also broadens the scope of labs’ QC activities beyond the analytical phase of testing. Overall, the expectation is that IQCP’s processes will help improve labs’ QC and resulting patient care.
“IQCP makes labs take into account preanalytics and postanalytics as a part of their QC program,” says Mears. “This means labs need to include everything from ordering the test to getting the result to the responsible provider.”
“The risk assessment approach to IQCP will definitely improve the quality of laboratory testing, since it encompasses all phases of testing—preanalytical, analytical, and postanalytical,” says Liggins. “This approach requires the laboratory to utilize all records and documentation in order to identify and evaluate the risk of errors in patient care. Such increased awareness of problem identification and mitigation will improve the overall quality and accuracy of testing, and ultimately improve the most important element, patient care.”
“If implemented and verified, the fundamental processes described in the Clinical and Laboratory Standards Institute’s EP23-A risk management guideline can reduce the number of laboratory errors by more than 50%,” agrees Brooks. “There would be millions fewer patients harmed and healthcare would save billions of dollars.”
While many labs are currently focused on performing the risk assessment activities that begin the IQCP process, the practical effects of the process are felt when labs implement practices to mitigate the risks their analysis has identified. “Using a risk assessment will allow a lab to have a better understanding of their potential for errors, and what specific actions they need to take to mitigate them,” says Olea.
“The goal of IQCP is to maximize the quality of lab results, and therefore optimize patient care and safety, with full consideration of the nuances and peculiarities of each lab’s individual practice and setting,” says Ng. “I know the weaknesses of my lab and healthcare setting for pre- and postanalytical issues, and my IQCPs will be focused on risk mitigation for things I know we can do better.
“The risks in my lab and healthcare setting may be completely irrelevant to another lab, and vice versa, so my IQCPs may be irrelevant (and perhaps nonsensical) to another lab,” Ng adds. “This is the beauty of IQCP—figuring out what doesn’t work in your own setting and fixing it. This is why ‘I’ is in IQCP, and why a one-size-fits-all approach for QC doesn’t work.”
Other lab leaders agree that IQCP’s mandate for labs to undertake risk assessments for each test, and each phase of each test, will bring about deeper understanding of a lab’s entire QC processes. Such awareness enables labs to focus resources on improved practices or training to minimize risks.
In spite of the potential that many lab leaders see for IQCP, others question whether the strategy will work for all testing sites. In some cases—especially in point-of-care settings—the processes involved in researching, developing, implementing, and operating an IQCP may require a lot of paperwork to produce a very small return on investment. In such cases, they conclude, the IQCP approach may not provide much help for improving QC among point-of-care instruments.
But IQCP may not be entirely without merit in point-of-care settings. “A risk-assessment approach that involves users allows them to start to understand what point-of-care coordinators are doing for them,” says Jenkins. “Also, it encourages point-of-care coordinators to understand what users are doing—not only for the coordinators, but also for the patient.”
EQC VERSUS IQCP
One of the major changes that will take place when the IQCP rules go into effect is that laboratories will no longer be permitted to use equivalent quality control (EQC) procedures to reduce their frequency of QC testing. Instead, labs seeking to modify their QC protocols will need to justify their changes by developing an IQCP. There are a number of major differences between EQC and IQCP, notes CRI’s Liggins:
- EQC used the same protocol for all applicable tests, regardless of their differences; IQCP is individualized for each analyte.
- EQC only applied to tests with internal QC mechanisms; IQCP can be implemented for all test specialties except pathology and its subspecialties.
- EQC was often performed to achieve acceptance of less QC; the objective of IQCP is to achieve more-effective QC, even if doing so requires an increase in QC testing.
- EQC was focused on the analytical phase; IQCP encompasses all three phases of the testing process.
- EQC is not risk-based and was not intended to promote risk reduction and mitigation; for IQCP, reducing risk is a fundamental goal.
“EQC had a narrower focus—centered primarily on the frequency and types of external quality controls for test systems,” says Ng. “My lab’s historical EQC practices demonstrated excellent test system stability. Where the quality of results fell apart was in how the specimen got to the test system (eg, mislabeled specimen, hemolyzed specimen) or in how the result was relayed to the provider (eg, lost transmissions, results displayed nonsensically in the electronic medical record).”
IQCP addresses such issues by requiring labs to assess and mitigate risks across all three phases of testing. “For IQCP, you’re not just using QC material to monitor quality,” says Olea. “You need to include elements that allow you to mitigate risk in specimens, reagents, the environment, test systems, and personnel. Because these are different for every lab, there is no one-size-fits-all model for a QC plan.”
“QC activities will be based on the risks of the individual lab,” agrees Mears, “and each lab will need to determine what the right QC activity is for them.”
The need to undertake such fiercely individualized planning has created some uncertainty about whether labs will find IQCP easier than EQC in the long run. “It’s comparing apples to oranges,” says Ng. “IQCP is more akin to a process improvement cycle. Labs have already been doing this for a long time. But IQCP is a way to cover all these activities under the umbrella of a single document so that the lab’s role in improving patient care is crystal clear.”
So far, compiling such a unifying document has been a challenge for labs. But there is hope that familiarity with IQCP processes will reduce labs’ administrative burden. “Once we get in the habit of writing our plans, it will become easier over time,” says Duke’s Nooney.
In addition, IQCP offers the opportunity to further streamline labs’ QC operations. “IQCP can be automated and centrally managed,” says Brooks.
Even so, the shift from EQC to IQCP represents a fundamentally new path for many laboratories, and more than a few labs are hesitating before setting out on the journey.
IQCP RESOURCES
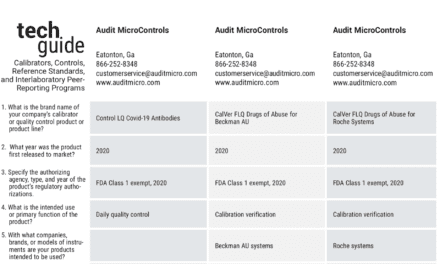
“There are many resources available, and a lab must take into consideration what their accreditor requires for IQCP, what their lab director needs to make a decision, and what works best for their lab,” says Olea.
Olea highlights resources accessible through Joint Commission Connect, a secure Web site for organizations accredited or certified by the commission. In addition to providing links to slide presentations and articles about IQCP, the site also includes a template that labs can use to complete their own risk assessment, and a sample completed IQCP.
In addition to professional organizations, government agencies and in vitro diagnostics manufacturers have also become sources of data used in creating an IQCP. “CMS guidelines and vendor offerings have been very useful,” says Jenkins. “When a vendor provides a templated plan that is prepopulated with its specific information, it saves time for the point-of-care coordinator.”
“All the vendors I have talked with have offered programs and resources,” affirms Nooney. “Spreadsheets from vendors with data about their individual tests have been very useful.”
STARTING TIPS
Labs may be behind schedule for implementing IQCP, but experts advise that with a little concentrated effort, they can still make January’s deadline. (For more information, see the companion article, “An IQCP Handlist.”)
“For laboratorians, understanding risk in the testing model is nothing new; they have been trained to identify and remediate risks as part of their routine duties,” says Liggins. “IQCP is an improved tool that will help them explore their processes, ask the right questions to better mitigate risks, and refine the skills they have been practicing all along. Labs should incorporate their past experience with a clear understanding of all the elements that IQCP covers, and seek out educational offerings to hone their skills.”
“As a first step, labs should reserve time to complete a risk assessment,” says Olea. “This task should not be overwhelming, since IQCP is in large measure simply formalizing what labs already know about their risks and the activities they currently perform to monitor quality. The key thing is to pick a format to use for a risk assessment and get started. The deadline is fast approaching, and labs’ time should be spent on developing their plans—not on learning how to use new tools.”
Labs may not be overwhelmed by the IQCP process, but that doesn’t mean it can be completed overnight. “It will take a lot of time and thought for a lab to write its plans,” says Nooney. “Labs should pick what they think will be the easiest test, start gathering the information they think they will need, and start writing. And then they should go back over it until they feel it is completed. If necessary, ask another coordinator to review the plan.”
“My lab is accredited by the College of American Pathologists (CAP), so what I found most useful is the flow diagram on the CAP website on how to get started with IQCP,” says Ng. “Specifically, labs should figure out which tests are not eligible for IQCP and remove them from their task list. Next, identify tests having external QC performed in accordance with CLIA regulations. If the lab doesn’t intend to change this external QC frequency, then there is no need for an IQCP. So the list of eligible tests will get shorter. Finally, identify the tests for which the lab is already applying EQC, or for which reduced frequency of external QC may be desirable. These are the tests for which the lab needs to start writing IQCPs.”
“Labs should start with areas that are currently using EQC,” advises Mears. “Also, when performing a risk assessment, labs need to think outside of the box—especially if other departments outside the lab are involved in the process.”
“At the least, the ability of the QC procedures to detect medically allowable errors should be evaluated,” says Brooks. “Read the glossary. Understand it yourself. IQCP makes sense.”
Whatever else experts may advise, the first message to labs is to get started. “Start now,” says Jenkins. “Start with what you are already doing. Write what you do, and make sure you do what you write.”
Steve Halasey is chief editor of CLP.











WHAT A BUNCH OF HORSE HOCKEY. IQCP ADDS MORE PROCEDURES AND VERBAGE TO EVERY LAB, THAT LABORATORIANS WILL NEVER READ. EXCEPT FOR THE POOR DIRECTORS, SUPERVISORS WHO HAVE TO WRITE IT, AND MAINTAIN THE RECORDS, AND RISK ASSESSMENT. LABORATORIES ARE ALREADY SPREAD TOO THIN, AND IF THE QA PLANS ARE ADEQUATE, IT ALREADY ADDRESSES ALL THE ISSUES BROUGHT FORTH WITH AN IQCP. I SUSPECT THAT LABORATORY INSTRUMENT AND SUPPLY COMPANIES HAVE HAD A MAJOR INFLUENCE ON THIS – WITH THE ADDED BURDEN OF INCREASED QUALITY CONTROL.
Hello James,
I know how you feel. I have been there, in the trenches, supervising and working side-by-side with my techs because there aren’t enough people. Now CMS wants to change the QC rules again? But this time, I agree with them. I know that the current state of QC and the quality of patient results is nowhere near what we need them to be. What can we do? We can start by simplifying QC, not making it more burdensome. We can check our QC processes and make sure they are doing what they are supposed to: catch problems with accuracy and precision before a bad patient result is reported.
There are several solutions out there. I would recommend the software from my friend and QC expert Zoe Brooks. It takes a few numbers from your current QC and tabulates current risk and potential risk (like EP23-A asks us to do). There are courses you can take at awesome-numbers.com to learn about these new concepts, how important they are, and what to do about them. Patients’ lives are at risk, and the costs of doing nothing are piling up. What if we could fix the QC problems and the costs of bad results? That would be a world I would want to work in.
In response to James Lay: That is exactly what IQCP is – unless the lab community uses this opportunity to make a real difference.
SQC reports a numerical indicator of the level of quality that is subject to errors of calculation and interpretation.
IQCP answers the question “Is risk acceptable” with a clear “Yes” or “No.”
The opportunity exists to make an exponential increase in QC effectiveness with minimal change to QC practice.
IQCP will be whatever we make, or sit back and allow, it to to be.
Zoe