AI-driven digital pathology can accelerate cancer diagnosis and clinical trial recruitment
By Simon Arkell and Dave Billiter
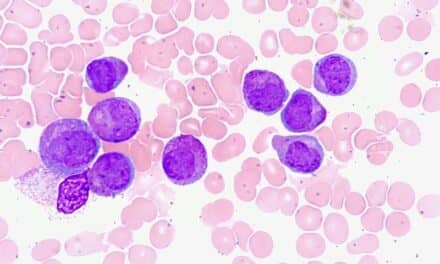
Pathologists play a number of critical roles as part of a patient’s medical care team. They oversee medical laboratories that perform a range of medical tests on a variety of sample types, such as blood, tissue, urine, or other body fluids, to make a diagnosis for the patient. Patient specimens may be configured to a glass slide for cytology and histology analysis under a microscope or tested through such molecular methods as real-time polymerase chain reaction (qPCR) or next-generation sequencing (NGS). Pathologists analyze and interpret such tests to determine the etiology, pathogenesis, and clinical significance of diseases, capturing their conclusions in detailed pathology reports (Figure 1).
Pathologists are trained to recognize hundreds of normal and diseased cell types and anatomical characteristics, but they face a significant challenge when it comes to staying abreast of new developments in the field. As a result of innovations in genomics, metabolomics, and proteomics, understandings of the biology associated with disease are increasing at rapid rate.
In everyday practice, an individual patient can be associated with numerous tissue and blood specimens and a multitude of data. In non-routine cancer cases, all this information is presented to a tumor board comprised of diverse medical professionals whose analyses inform the patient’s diagnosis and treatment plan. Often these experts are faced with a tsunami of information that is relevant to the patient’s diagnosis and treatment plan and is also important for determining the patient’s eligibility to participate in a clinical trial.
Clinical Trial Eligibility
Clinical trials are run by pharmaceutical companies during drug development to assess the safety and effectiveness of novel therapeutics or interventions. An early step in clinical trial design involves establishing eligibility criteria so that it can be determined whether patient volunteers meet trial requirements.
Identifying patients with a specific diagnosis and matching them to a clinical trial can be a challenge. Acting as the sponsor, the pharmaceutical company can recruit patients directly, or it can work through a contract research organization (CRO), principal investigator (PI), clinical research coordinator (CRC), or patient advocacy group.
While pathologists sit on the care team and are involved in making a patient’s diagnosis, the process of running tests and reviewing findings in order to arrive at a diagnosis can be fragmented, and the turnaround time can be lengthy. Moreover, information about suitable clinical trials specific to each patient’s diagnosis may not be readily accessible.
Improvements to the pathology workflow through the application of artificial intelligence (AI) can improve the efficiency of clinical and research processes, while also connecting eligible patients to clinical trials at the time of diagnosis. Such AI-enhanced approaches benefit patients by expanding access to therapeutic alternatives, and benefit trial sponsors by accelerating trial enrollment timelines.
Clinical Trial Recruitment Process
The process of running a clinical trial involves many phases and medical professionals. In research institutes and other clinical settings, the key figure in managing the operation of a trial is the PI, who may also be a practicing physician involved in treating patients.
When an oncologist performs a biopsy on a patient, the tissue is sent to a pathologist for diagnosis. That diagnosis is indicated in the pathologist’s report, which is attached to the patient’s electronic medical record (EMR) and sent to the oncologist. If the oncologist is also serving as PI for one or more clinical trials, they may be aware of a trial that is suited for a specific patient.
In parallel, both PIs and CRCs use clinical trial management systems to gain visibility into the availability and suitability of clinical trials for patients known to them. They search EMRs and other systems, filtering through the inclusion and exclusion criteria associated with each trial, to identify patients that could be enrolled. If they find a match, they contact the PI.

Table 1. Data detailing the market demand and actual performance for enrolling clinical trials indicate that biopharmaceutical sponsors are struggling to find patients and fill trials.
The process of recruiting patients for clinical trials remains a time-intensive, costly barrier to the execution of drug development programs. Providers and institutions may not be aware of studies for which a patient may be qualified. In the field of oncology alone, more than 14,000 clinical trials are currently recruiting patients, yet the rate of participation by potential trial candidates is estimated to be as low as 3%.1,2 Consequently, pharmaceutical companies must invest heavily in patient recruitment activities, trying to build networks of trial sites that have specific patients with specific diseases.
Pharmaceutical company sponsors typically contract with a CRO to find and inform study sites about their trial and to look for patients who may be a match. Even when a potential match is identified, however, the patient may not meet some of the critical inclusion or exclusion criteria, such as failing a first-line treatment, receiving a specific class of drugs, or having undergone a specific molecular diagnostic test. Such mismatches can disqualify a patient for a trial.
Considered on a grand scale, such mismatches also make clinical trial enrollment time-consuming and expensive. In 2017, the patient recruitment market was valued at $4.8 billion, and it is projected to grow at a compound annual growth rate of 15% to 16% through 2020.3 In fact, 48% of sites underenroll study volunteers, and most trials end up doubling their original timelines to meet enrollment goals (Table 1).4 Competition for patients is steep, awareness is low, and the time for matching treatment options to the patient is critically limited.
The Big Data Problem
The prevalence and complexity of cancer are continuing to increase demands on pathologists at a time when most observers expect that the number of available pathologists is likely to decline substantially.5 This means a heavier workload for an already busy profession. In order to spend time on important elements of the diagnostic process without reducing the quality of their work, pathologists need workflow improvements that can automate many of their basic tasks.6
In many large hospitals, efforts to digitize microscopy through the use of whole-slide image scanners have been successful. Nevertheless, for the purpose of identifying patients with a diagnosis that would make them eligible for a clinical trial, efforts typically rely on data coming from the patient’s EMR.
For patients, oncologists, PIs, and CRCs, the challenge of sifting through EMRs and various trial descriptions to find a match can be considered a ‘big data’ problem. The data are available, but the process of aligning and matching patients to trials is highly inefficient. What’s needed is a new mechanism that quickly aggregates data to help pathologists make diagnoses and enables sponsors to match patients to trials. The result should be not only to fill trials more quickly but, more importantly, to expand therapeutic options that may positively affect patient outcomes.
An Innovative Digital Pathology Cloud Platform
An AI-driven digital pathology Cloud platform has recently been introduced to enhance pathology workflows, peer-to-peer collaboration, and patient identification for clinical trials. Developed by Deep Lens Inc, Columbus, Ohio, the Virtual Imaging Pathology for Education and Research (VIPER) platform supports pathology teams in confirming a patient’s diagnosis and advising clinicians about the patient’s potential eligibility for a clinical trial.
VIPER is a workflow solution designed to process pathology cases more effectively by digitizing images and associated data. It draws on thousands of cases with digital images, associated annotations, and diagnoses that have been uploaded by pathologists over the past 10 years (Figure 2). When a new image is introduced, VIPER scans stored images and, using machine learning, recognizes and presents cases with high similarity. To help in confirming a diagnosis, data associated with stored images highlight such key diagnostic features as percent mitosis, mitotic index, and anaplasia. VIPER’s logic-based workflow also presents new biomarker information, new stains, and assays relevant to clinical trials that the pathologist may not know about. The different facets of data that VIPER consumes are presented at a patient level in a user-friendly graphical interface.
Early adopter Jason A. Jarzembowski, MD, PhD, assistant professor of pathology at the Medical College of Wisconsin and director of the perinatal pathology program at Children’s Hospital of Wisconsin, welcomes the technology interaction. He cites especially VIPER’s ability to automate cell counts, enumerating total cells, mitotic cells, and the fraction positive or negative, and discerning between nuclei and cytoplasm staining. Counting 5,000 cells now takes 2 milliseconds instead of 20 minutes. For Jarzembowski and other pathologists, automating such time-consuming tasks frees them up to do more important work. More importantly, it’s not error-prone like humans. For Jarzembowski, the key benefit is that VIPER can’t be swayed toward a certain diagnosis.
An Accurate Diagnosis
VIPER creates robust workflows that mimic activities a pathologist conducts with a microscope. Using AI and leveraging innovations in scanners, software, and next-generation algorithms, VIPER can rapidly sift through different cases, images, and features of tumor types analyzed by other pathologists, surfacing information not previously available to aid in making a more accurate diagnosis.
In a recent study, VIPER was applied to classification, segmentation, and detection tasks on publicly available benchmark datasets and compared with existing machine learning approaches (Table 2).7 For classification of the lymphoma subtypes chronic lymphocytic leukemia, follicular lymphoma, and mantle cell lymphoma, VIPER achieved 99.8% testing accuracy and 3.22% better performance than existing approaches. For classifying invasive ductal carcinoma, VIPER achieved 89.07% testing accuracy and 4.39% better performance.

Table 2. Data comparing VIPER to existing machine learning approaches for analyzing publicly available benchmark datasets applied to classification, segmentation, and detection tasks.
In the segmentation tasks, the experimental results showed that VIPER achieved 6.5%, 3.31%, and 4.13% better performance for epithelium, nuclei, and tubule segmentation, respectively, compared to existing approaches. For lymphocyte detection, VIPER achieved 90.92% testing accuracy and achieved around 0.82% better performance. Mitosis detection revealed 97.32% and 60% testing accuracy for image-level and patient-level respectively. The experimental results demonstrate the robustness and efficiency of VIPER for different use cases of computational pathology.
Because VIPER supports secure remote login, pathologists can share cases and consult with experts about rare tumors, facilitating collaboration and nuanced cancer diagnoses. All diagnoses are saved into VIPER and are searchable for future reference to benefit other pathologists and patients.
At the Columbus Children’s Research Institute, physicians had a complex quality control (QC) process which required that glass slides and paper forms be physically shipped to consulting pathologists at other institutions. That process resulted in extended QC review times and substantial shipping costs. VIPER simplified this process through its Web-based pathology review and digital archive of original pathology material.8 According to Jarzembowski, the new process is no different from walking down the hall to consult with a colleague. Now, he’s just using a computer to facilitate the conversation.
For the patient, reduced time to diagnosis means faster access to treatment. Moreover, an accurate diagnosis means greater assurance for treatment fit.
Window of Opportunity for Trial Eligibility
By enhancing clinical trial recruitment, VIPER creates a new window of opportunity to intervene with a patient much earlier than the current process permits. Clinical trial designs can be married to the innovative operational acumen of VIPER. When used at an institutional level, VIPER can surface information associated with trials through real-time diagnosis, alerting and enhancing coordination among research teams, care teams, and patients.
To this end, Deep Lens is partnering with Worldwide Clinical Trials (WCT) to shorten recruitment and development timelines for oncology trials. WCT is a global CRO that helps biopharmaceutical sponsors access hard-to-find patient populations and manage the complexities of oncology clinical trials.
The partnership supports coordination between care teams and patients for trial recruitment by presenting clearer treatment and clinical trial options earlier in the process. With VIPER, when the pathologist informs the treating oncologist about the biology and the nature of the disease, they can also convey information about potential trial-related activities that may be pursued.
This novel protocol elevates the pathology discipline by making the pathologist the primary source for identifying relevant clinical trials at the earliest stage—the time of diagnosis. Because this information is available earlier, action can be taken sooner, commencing the process of enrolling in a clinical trial before the patient is put on standard of care or a competing therapy.
VIPER Access for Pathologists
Hospitals and pathology labs can now participate in sponsored trials by identifying patients and offering expanded treatment options for patients. Deep Lens offers VIPER free of charge to pathology groups worldwide, enabling them to enhance their workflow, contribute cases to clinical trials, and improve patient diagnoses. Users have access to fast and accurate information and expert consultation to help optimize patient care and support clinical research. Digitized slides are dynamically uploaded to the Deep Lens Cloud server and images are available for viewing within 2 days. Additional storage and AI capabilities incur a small monthly fee.
Conclusion
Given the time-critical nature of cancer and the thousands of clinical trials with varying eligibilities, there is a need to match patients to trials more quickly—at the time of diagnosis whenever possible. AI-driven digital technology can affect outcomes and bring clarity and confidence to the challenging moment when patients are first diagnosed. Deep Lens is leveraging machine learning and Cloud-based platforms to accelerate image analysis, improve accuracy, and support collaboration. When patients, pathologists, physicians, and trial sponsors work together with immediate access to diagnoses, treatments, and trials, patients can receive better care.
Simon Arkell is president and cofounder and Dave Billiter is CEO and cofounder at Deep Lens Inc. For further information, contact CLP chief editor Steve Halasey via [email protected].
References
- ClinicalTrials.gov [online]. Bethesda, Md: National Library of Medicine, 2019. Available at: https://clinicaltrials.gov. Accessed September 9, 2019.
- Institute of Medicine Forum on Drug Discovery, Development, and Translation. “Clinical Trials in Cancer.” In:Transforming Clinical Research in the United States: Challenges and Opportunities: Workshop Summary (Chap 6). Washington, DC: National Academies Press, 2010. Available at: www.ncbi.nlm.nih.gov/books/NBK50895. Accessed September 9, 2019.
- Ilancheran M. Analyzing the top clinical trial outsourcing trends of 2017 [online]. Clinical Leader. December 28, 2017. Available at: www.clinicalleader.com/doc/analyzing-the-top-clinical-trial-outsourcing-trends-of-0001. Accessed September 9, 2019.
- Lopienski K. Challenges in patient recruitment: how to prevent under-enrolling clinical trials [online]. Madison, Wis: Forte, 2018. Available at: https://forteresearch.com/news/challenges-patient-recruitment-prevent-enrolling-clinical-trials. Accessed September 9, 2019.
- Robboy SJ, Weintraub S, Horvath AE, et al. Pathologist workforce in the United States: I. development of a predictive model to examine factors influencing supply. Arch Pathol Lab Med. 2013;137(12):1723–1732; doi: 10.5858/arpa.2013-0200-oa.
- Cancer, pathology, and the law of supply and demand [online]. Philadelphia: Proscia, 2018. Available at: https://proscia.com/cancer-pathology-and-the-law-of-supply-and-demand. Accessed September 9, 2019.
- Alom MZ, Aspiras T, Taha TM, et al. Advanced deep convolutional neural network approaches for digital pathology image analysis: a comprehensive evaluation with different use cases [online]. Ithaca, NY: Cornell University, 2019. arXiv:1904.09075v1 [cs.CV]. Available at: https://arxiv.org/pdf/1904.09075.pdf. Accessed September 9, 2019.
- Ramirez NC, Barr TJ, Billiter DM. Utilizing virtual microscopy for quality control review. Dis Markers. 2007;23(5–6):459–466; doi: 10.1155/2007/959376.